Short answer
Electroshock therapy is a very effective and safe treatment for a number of psychiatric disorders. With this therapy, small electric shocks are given to the brain, which generate something that resembles an epileptic seizure. This technique has existed for almost a hundred years and is used worldwide, including in the Netherlands, in order to treat people with severe depression. The effects of ECT are clearly visible in clinical practice, with several theories about the underlying mechanism of action. Both animal experimental research and brain scans of people before and after ECT show a possible growth of the number of brain cells and connections in the brain.
Longer answer
One Flew Over the Cuckoo’s Nest: an outdated image
It is possible that the notion of electroshock therapy brings up gruesome images of Jack Nicholson in the blockbuster “One Flew Over the Cuckoo’s Nest”. Playing the role of ‘Randle’, who ends up locked up in a psychiatric institution, he is declared insane, tied up, and treated with electroshock therapy against his will to calm him down. The film ends even more poignantly: with a lobotomy (a very controversial method in which part of the brain is removed. Lobotomies have of course long since been discontinued). The last ‘medicine’ to suppress him and control his mind seems to have finally worked!
Electroshock therapy used in clinics is usually called electroconvulsive therapy (ECT). The dramatic and outdated interpretations of electroshock therapy (‘One Flew Over the Cuckoo’s Nest‘ is 50 years old!) contain strong fictional elements that do not comply at all with the appropriate use of this everyday practice. ECT is used as for cases such as severe depression, therapy resistant schizophrenia and catatonia (a condition in which a person becomes less able to respond to his or her environment; for example, by remaining still and unresponsive). Psychiatric patients receive ECT in the two following cases: (1) when neither cognitive therapy (sessions with a psychologist) nor medicine such as antidepressants (to treat depression) or clozapine (to treat schizophrenia) seem to work or are not well tolearted (2) in rare cases involving people who are very seriously ill or pose an acute danger to themselves or others.
Treatment
Most patients come in for treatments twice a week at one of the thirty clinics in the Netherlands that offer ECT sessions (some patients are admitted for a variety of reasons). These sessions are short: the treatment itself takes about 20 seconds, where short electric shocks of about 0.9 ampere (the strength of a bicycle light) are administered via electrodes stuck to the head. In the Netherlands, patients are always sedated and given muscle relaxants, so that no muscle convulsions (cramps and shocks throughout the body) occur. Furthermore, a slew of measuring equipment (including an electrocardiogram (ECG) to measure the heart activity) and a crew of medical professionals (including an anaesthesiologist to oversee the sedation) see to it that all proceeds safely. After about twelve sessions (spread out over six weeks), the treatment is completed.
Side-effects
While ECT is safe, there are some known, mostly temporary, side-effects. Patients may experience a brief period of confusion, which often resolves within an hour of an ECT session. It does occur that patients have memory complaints. During the treatment period, patients may have difficulty creating new memories (anterograde amnesia). It is not that memory disappears, but rather that no new memory is created. However, it can also happen that memory from before the treatment is affected (retrograde amnesia). People struggle for instance to recall their (recent) 40th birthday or their wedding day. This can of course be experienced as very disturbing and also painful. Fortunately, most memories return after the ECT sessions, and some memories are never affected. It is not the case that people forget how to brew a cup of coffee for instance. It is not yet fully understood how much of these side-effects are caused by the ECT itself and how much are due to both the temporary sedation that patients receive during these treatments (to prevent convulsions) and the effects of a severe depression on the brain.
Despite the safety and efficiency of this technique, ECT still has its ‘bad rep’. In persistent depression (a depression that lasts longer than two years), ECT is strongly recommended by national guidelines. Although 26% of patients with a persistent depression are eligible for ECT nationwide, the treatment method is only used in 1% of this group. A worryingly small percentage. This seems to be due to both a lack of knowledge and referrals within the medical world as well as the choice of patients themselves. At the moment, the recent (re)discovery of ketamine is more popular for the treatment of depression and some patients even prefer deep brain stimulation (an effective, but also invasive treatment treatment in which electrodes are placed inside the brain). All this, in spite of the fact ECT has been used for about a hundred years and is very successful with a response rate between 50-80% (depending on several factors).
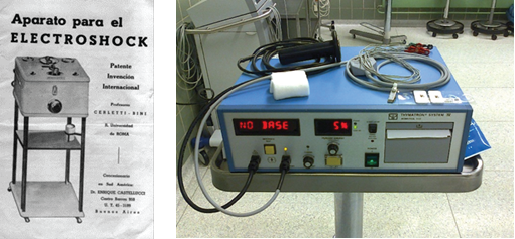
Left: The original machine, by Ugo Cerletti and Lucio Bini, used for the first ever ECT treatment in humans. The machine stands in the Museo di Storia della Medicina (Museum of Medical History) of the Sapienza University in Rome. [image from Alessandro Aruta, Museum Curator – Sapienza University]. Right: An example of a modern ECT machine, where precise amperage and frequency can be calibrated by medical professionals. [https://nl.wikipedia.org/wiki/Elektroconvulsietherapie].
The invention of the ECT goes back to the early 30s of the last century and is mostly based on the work of an Italian neurology duo. Ugo Cerletti and Lucio Bini were observing how pigs received an electric shock before they were slaughtered and it calmed them down. After extensive animal research in order to optimize the parameters for the ECT, they developed their first, safe machine in order to treat humans, and quickly already noted positive effects after 10-20 sessions. The technique has been adapted over the years (for instance, the inclusion of sedation and muscle relaxants) and, at this moment, a million people are being treated with ECT every year, worldwide.
Mechanism
But how does ECT actually work? What exactly is the effect on the brain? In severe depression, brain cells die and the connections between these cells also decrease; this affects the network in our brains. In animals (often rats and mice are used for this type of research), these connections increase again after ECT and new neurons are even created (a process called neurogenesis). In humans, it is more difficult to investigate the effect of ECT on the brain. However, when researchers compare brain scans (MRIs) of patients before and after treatment, they see a subtle growth of brain areas such as the hippocampus (4-5% growth) and the amygdala (5-6% growth). What this growth exactly means and whether it corroborates either the results of animal experiments on a cellular level, or the positive effect it has on groups of patients, is currently being investigated.
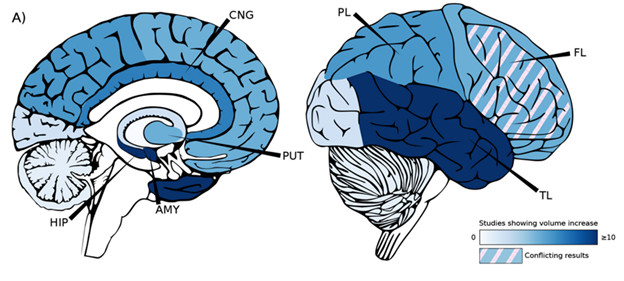
When you compare patient MRI scans from before and after ECT, there are a number of brain areas where the grey matter (neurons) volume has increased. The image above shows a summary of a large number of studies researching the increase in grey matter. Growth is mostly seen in the Hippocampus (HIP) and the Amygdala (AMY). Other areas such as the Putamen (PUT), the Cingulate Gyrus (CNG) and the Parietal, Frontal and Temporal Lobes (PL, FL and TL) show less growth. This image is sourced from an article by Ousdal and colleagues: [10.1016/j.biopsych.2021.05.023].
In clinics worldwide, electroshock therapy, or ECT, is not only still used; it is actively being developed. ECT remains one of the most effective and safe treatments for severe depression and schizophrenia. Unfortunately, this method has (unjustly) gained a bad reputation which, in time, can be detrimental to people who could greatly benefit from this treatment. The ‘Randle’, in real life, is much less sensational. He is not locked up against his will, stuck in a psychiatric ward with tormentors. He (or she), drives to the clinic once or twice a week for a voluntary, short treatment to rid himself (or herself) of the tormentors in his (or her) head.
Read more?
(Dutch) https://www.hersenstichting.nl/behandelingen-van-hersenaandoeningen/elektroconvulsietherapie-ect/
Ousdal, O. T., Brancati, G. E., Kessler, U., Erchinger, V., Dale, A. M., Abbott, C., & Oltedal, L. (2022). The neurobiological effects of electroconvulsive therapy studied through magnetic resonance: what have we learned, and where do we go? Biological psychiatry, 91, 540-549.
Scheepens, D. S., van Waarde, J. A., Lok, A., de Vries, G., & van Wingen, G. A. (2020). The link between structural and functional brain abnormalities in depression: A systematic review of multimodal neuroimaging studies. Frontiers in psychiatry, 11, 486702.

