Short answer
How Alzheimer's disease develops is a very challenging question to answer, as the disease manifests in so many different ways! Ultimately, the build-up of harmful molecules in the brain triggers a complex process of deterioration, which leads to the debilitating symptoms of Alzheimer's, such as dementia. While genetic risk factors play a role, they are not decisive. Maintaining a healthy lifestyle – as is often the case – provides some hope for reducing the risk of Alzheimer's. This includes regular physical activity, balanced nutrition, sufficient sleep, and consistently engaging in new learning experiences.
Longer answer
A combination of causes
Alzheimer’s disease (or in short: Alzheimer’s) is a highly complex condition, with as many explanations for its onset as there are patients suffering from the disease. The pathology of Alzheimer’s disease is heterogeneous (meaning it comprises different types) – no two individuals develop the disease in the same way. This variation implies that the underlying causes or ‘triggers’ differ from one person to another.
Broadly speaking, Alzheimer’s disease begins with the accumulation of toxic molecules both within and around the brain’s cells. Over the course of 10 to 20 years, this build-up gradually leads to the clinical symptoms of the disease, with memory loss (a form of dementia) being the most prominent. (Quick note: dementia is not the same as Alzheimer’s disease; it can also be a symptom of other neurological conditions, such as Parkinson’s disease.)
For years, the prevailing view was that Alzheimer’s disease resulted from the death of neurons, which are among the brain’s most important cells. Neurons have long been regarded as the brain’s primary ‘actors,’ and this notion shaped much of the earlier understanding of Alzheimer’s. However, technological advances and genetic research have revealed a more nuanced picture. Alzheimer’s disease is not solely the result of a single cell type failing. Instead, it arises from a complex interplay between various cells and systems that gradually deteriorate.
This deterioration initially disrupts everyday activities (Where did I put my keys?) and, over time, leads to the complete loss of memory and even identity. The complexity of the disease – and the range of molecular and cellular changes accompanying it, such as inflammation and the loss of connections (synapses) between neurons – results in the many different phenotypes (the sum of all observable characteristics) seen in people with Alzheimer’s disease. So, can we truly call Alzheimer’s a single disease? Not really. This diversity also presents one of the greatest challenges in developing effective treatments that work for large groups of people.
Genes and environment
Returning to the original question: What determines how and when someone develops Alzheimer’s disease? One key factor lies in our genes: everyone carries some level of risk based on their genetic makeup. There are hereditary forms of the disease, caused by mutations in specific genes, that can lead to Alzheimer’s at an earlier age. However, these cases represent only a tiny fraction of all Alzheimer’s patients (less than 5%). What about the risk for the vast majority of Alzheimer’s patients who develop the disease later in life? The risk can be likened to driving a car without wearing a seatbelt. This increases the likelihood of injury, but only if a crash occurs. In this analogy, the ‘crash’ represents environmental factors and additional health conditions. The silver lining? In non-hereditary Alzheimer’s disease, you can always choose to ‘put on the seatbelt.’ By staying physically active (e.g., through exercise and a healthy diet) and mentally engaged (e.g., learning a new language or skill or solving puzzles), you can lower your risk throughout your life.
Damage
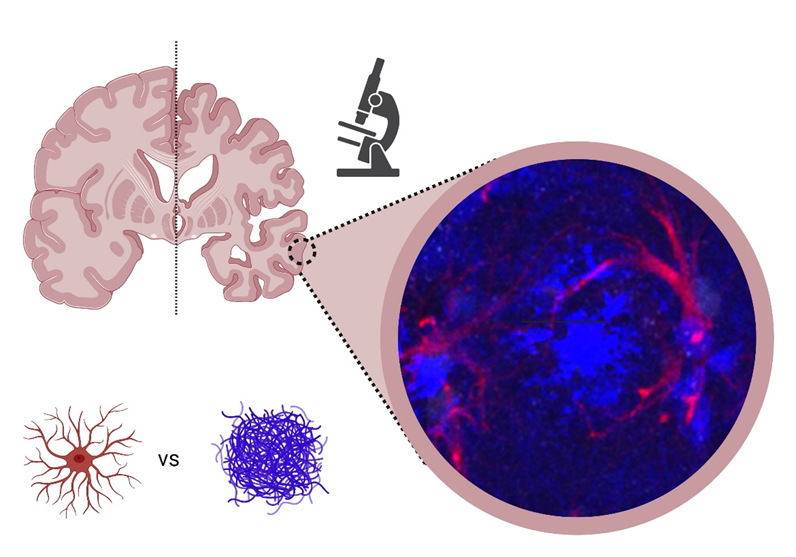
The brain damage caused by Alzheimer’s disease is clearly visible in the image above. On the left is a schematic representation of a healthy brain hemisphere, and on the right is the hemisphere of someone affected by Alzheimer’s disease. Microscopic examination reveals how brain cells attempt to clear harmful accumulations of molecules (shown in blue and referred to as plaques). A key type of brain cell involved in this process is the astrocyte (highlighted in red). Astro = star in Greek, reflecting the cell’s star-like shape. The inset shows a microscopic image of astrocytes from mouse brains actively engaging with plaques. This image was provided by Sarah Snoeck from Evgenia Salta’s lab at the Netherlands Institute for Neuroscience.
Reserves
What happens when toxic accumulations continue to build up in the brain? Does this inevitably result in dementia and further cognitive decline, such as difficulties with memory, language, intelligence, and concentration? In short – does one necessarily lead to the other? Recently, the well-known story of Alzheimer’s has taken an unexpected turn. Researchers have discovered that 30% of elderly individuals, upon post-mortem examination, show Alzheimer-related changes in their brains. Surprisingly, many of these individuals displayed no cognitive impairments during their lives!
How is this possible? The brain is a remarkably resilient organ, capable of building cognitive reserves over a lifetime. These reserves can act as a buffer against dementia, even when Alzheimer-related changes are present. So, how can these reserves be developed to slow or even prevent cognitive decline? Unfortunately, there’s no single solution – no magical fix! While genetics do play a role, the most effective way to build reserves is to live a life in which you are constantly seeking new challenges and learning new things.
Read more?
(Dutch) Voor een toekomst zonder dementie | Alzheimer Nederland (alzheimer-nederland.nl)
(Dutch) Dementie.nl: Alles over omgaan en leven met dementie
Alzheimer’s Association | Alzheimer’s Disease & Dementia Help
ALZFORUM | NETWORKING FOR A CURE
https://nin.nl/research-groups/salta/

